By your late thirties or early forties, you may be noticing some big changes going on in your body.
This phase is called perimenopause and marks the ending of your reproductive years.
Here, we discuss what perimenopause is, the 4 main stages and what can affect the transition period to perimenopause.
Perimenopause is a sequence of events
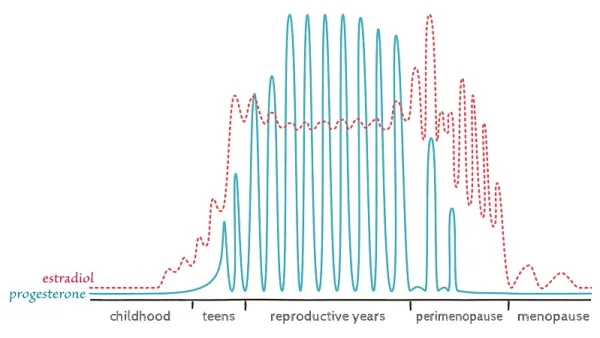
Perimenopause is a transition phase of life prior to menopause – where a woman’s ovaries stop producing eggs and the production of hormones such as estrogen and progesterone decline.
However, perimenopause is NOT just one event and menopause does not occur suddenly.
There are actually 4 main stages in perimenopause:
- Very early menopause – first 2-5 years beginning with a gradual decrease in progesterone and high oestrogen.
- Early menopause transition – marked by the onset of irregular periods and oestrogen is wildly fluctuating.
- Late menopause transition – marked when you miss your first period, this phase is when oestrogen becomes low and lasts around 4 years.
- Late perimenopause – This is your countdown until menopause, i.e. the date marked from your last period until the 12 months following.
This is something that we go into depth in our perimenopause support program, Thrive After 35.
What affects the Transition Period?
So, how can we guarantee a smooth transition period in perimenopause?
There are so many factors affecting how well you transition into perimenopause and beyond. Some of these are set in stone, however, there are diet and lifestyle factors which are modifiable as well.
Below are some of the factors affecting the transition period of perimenopause (maybe change)
- Genetics
Genetics plays a strong role both in the timing of menopause and even the severity of symptoms in some degree (1).
It may be a good idea to ask your female family members their experiences of perimenopause, as this may give you a bit of an insight as to what to expect.
However, the expression of these genes is equally, and if not more important to the genes themselves. The expression of these genes is affected by your nutrition, lifestyle, movement and sleep.
- Your general health prior to perimenopause
Explained well by Lara Briden – “Perimenopause is like a barometer of health” (1).
Any health issue that was a problem prior to perimenopause, you can expect to bring to the surface and be amplified during this time.
Essentially, this means that the best treatment for your particular perimenopausal symptoms is often the treatment you needed in the first place.
- Your period health prior to perimenopause
Symptomless periods and menstrual cycles can most likely predict a smooth sailing transition into perimenopause.
However, as general health concerns are amplified throughout perimenopause, so are symptoms surrounding your menstrual cycle.
This is because symptomless periods are often a good indication that your hormones are balanced and working well. Particularly, it is important to ensure that your body can clear and metabolise oestrogen whilst your brain can accommodate these changes (1).
- Medical conditions
There are certain conditions which may contribute to an earlier onset of perimenopause. Examples of this include rheumatoid arthritis (RA), epilepsy or thyroid disease (1).
It should be noted that certain medical treatments such as hysterectomy, removal of the ovaries, chemotherapy or radiation will bypass perimenopause and enter a ‘forced’ medical menopause (1).
- Lifestyle factors
Although perimenopause is an inevitable stage of life for women, there are certain controllable factors that can affect the severity of symptoms and when you enter perimenopause (2).
- Smoking – there is some evidence to show that smoking can bring on perimenopause up to 2 years earlier and increase severity of symptoms.
- Alcohol consumption – alcohol can trigger hot flushes and other perimenopausal symptoms.
- Regular exercise – maintaining regular exercise can help to reduce hot flushes and night sweats. Additionally, exercise has endless benefits including improved cognitive functioning, reduced depression and fatigue, strengthens bones, aid in healthy sleep, and maintain weight.
- Relaxation and/or yoga – relaxation practices such as yoga, meditation and deep breathing may help reduce feelings of anxiety and depression as well as managing sleep disturbances.
Thriving for the Long Term
So, how can you set yourself up to thrive in perimenopause and beyond?
This information may be overwhelming, however, we won’t leave you in the dark.
If you want to learn more about this transition period and thrive through the process, join the waitlist to our perimenopause support program, Thrive After 35, so that you can thrive in your health for life.